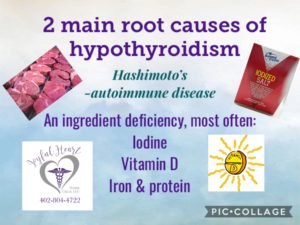
Vitamin D is called a vitamin; it’s often called a hormone. It’s often called a vitamin that acts like a hormone. So, which is it? It’s actually all of the above. Vitamin D is a fat-soluble agent with a chemical structure similar to a steroid. Which makes sense, as Vitamin D is one of the major ingredients of all steroid-based hormones produced in our bodies. Our bodies were created and designed to absorb sunshine via skin and then a variety of chemical reactions would occur so our bodies actually made its own vitamin D. However, since the skin cancer scare of the 1970s, the general population applies thick layers of sunscreen and we rarely remove enough clothing to bare our skin for this natural process to occur. This long-term lack of sunshine on our skin is producing entire generations of significantly deficient people in our society.
What happens when we are low in vitamin D? How does a vitamin D deficiency affect people’s health? Because vitamin D is vital to numerous human processes, it can be quite complex to discuss its actions, roles, and benefits to our bodies. We will attempt to explain vitamin D as simply as possible, describing the intricacies and complex utilization of vitamin D.
The oldest known function of vitamin D is the role in bone growth and development; we’ve all seen photos of young children with rickets (legs bowing outward) because of a severe deficiency of vitamin D. Without adequate D in the bloodstream, bones cannot grow or develop properly. For years, calcium was reported to be the “hero” of the skeleton. People with weakening bones were urged to take high doses of calcium daily “to protect your bones” and prevent osteoporosis. However, in recent years, that advice has been scaled back a bit; no longer is it general health advice to recommend calcium supplementation unless there is known osteoporosis or osteopenia. Even where there is evidence, many providers won’t recommend it lightly; they take great care in explaining the risks/benefits and often encourage vitamin D in place of or at least along with the calcium. So, just what does the vitamin D do for bones? It’s most recognized benefit is that it aids absorption of calcium from the intestines; it’s the reason vitamin d is added to milk and other dairy products. Milk/dairy products do NOT naturally contain vitamin D; it is added to promote calcium absorption into the bones for effective use in growth & development. Vitamin D helps keep bones strong and also helps prevent weak, brittle bones in the elderly.
In addition to bone health, vitamin D is recognized for its effects in the brain; it has been called “the depression vitamin” among health care professionals for many years because it is a vital component of neurotransmitters in the brain. Three major neurotransmitters in the brain requiring adequate amounts of vitamin D include serotonin, oxytocin, and vasopressin; serotonin is a neurotransmitter vital for transmitting nerve impulses. Serotonin is also important for mood regulation; pain perception; gastrointestinal function, including perception of hunger and satiety; and other physical functions. Oxytocin is released from the brain when it is needed for a variety of body needs, including labor & delivery at the end of pregnancy, during sexual arousal, and it is often referred to as “the love hormone” because of its impact on emotional relationships. Vasopressin is an anti-diuretic hormone that regulates fluid balance within the body and bloodstream. It works to prevent excess fluid loss and helps maintain homeostasis (normal internal chemistry) by maintaining the concentration of dissolved particles, such as salts and glucose, in the blood. Reviewing all 3 of these neurotransmitters and their major functions is vital to understand brain chemistry; can you see how a shortage of vitamin D would impact nearly all normal body functions and even our relationships, moods, and emotions?
Vitamin D’s impact on glucose has only recently been identified; multiple studies show conflicting data as this area is new to research. However, knowing that vitamin D is an essential ingredient of vasopressin, and that vasopressin helps maintain healthy glucose concentrations, does it not then make perfectly logical sense that a shortage of vitamin D will result indirectly or directly in elevated glucose levels?
In addition, a recent study shows that fasting glucose levels, insulin levels and insulin resistance all improved with vitamin D supplementation. Additionally, this study suggests that pro-inflammatory cytokines that are thought to contribute to insulin resistance were down-regulated with this vitamin D supplementation. Translation: with high carb/high sugar intakes, we are finding significantly elevated levels of inflammatory markers, like cytokines, that are more linked to heart disease, heart attacks and strokes than we ever imagined. Vitamin D supplementation appears to reduce that inflammation as part of the body’s normal healing/tissue repair processes.
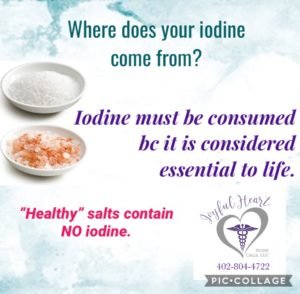
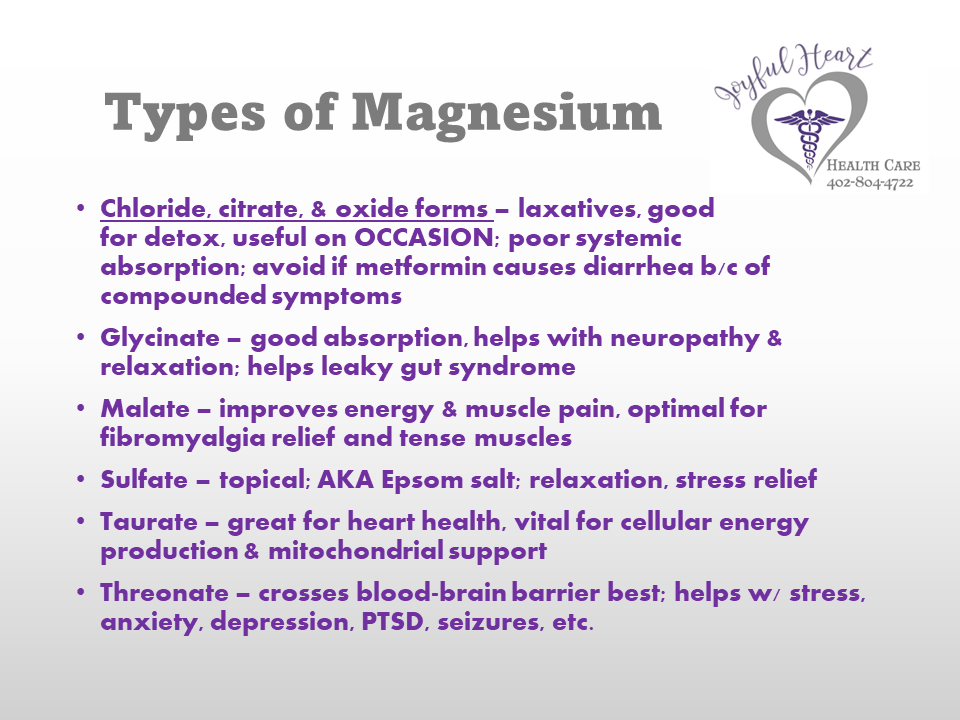
However, let’s review again: former advice to take calcium for bone health came with advice to also take vitamin D to aid absorption of the calcium. Just as calcium needs vitamin D for absorption & effective utilization, so vitamin D needs some help. Magnesium, iodine, healthy fats, and vitamin K2 are necessary for the absorption and use of vitamin D. Recent studies have shown even the very high doses of vitamin D prescribed by health care providers (50,000 IUs) as a weekly regimen barely raised vitamin D levels at all after 4-6 weeks, the usual recommended time frame for dosing. Once study participants added a magnesium and/or vitamin K supplement to their regular dosing regimen, vitamin D levels immediately began to rise. These studies are why we typically recommend vitamin D, magnesium, fats, iodine, and vitamin K2 for most people with insulin resistance and type 2 diabetes.
Recently some reports are suggesting that vitamin D is integral to our immune system; some experts and studies are recommending to add or increase vitamin D supplementation during a variety of illnesses, including colds, flu, respiratory illness, asthma, and more.
What about doses of these supplements? There are limited studies and recommendations because this field is so new and mainstream medical providers are hesitant to make recommendations to patients without a large body of support. The Endocrine Society has stated that a deficiency of vitamin D exists when lab levels fall below 20 ng/mL; however, many reputable experts and organizations say that level should be 40 or even 50 ng/mL. Because of limited evidence, it’s difficult to specify a particular dose. Even more recently, various mainstream medical organizations like the Endocrine Society have stated that health care providers should not draw a vitamin D level on patients anymore, because we’re all deficient anyway, & the test is very expensive; most insurances won’t cover the costs either. So how are we supposed to know what dose to take? Well, the current recommendations for dosing are not clear and without a known vitamin D level, finding your perfect dose may be tricky, but many people find that 1,000 – 2,000 IUs daily is a good maintenance dose; some people just beginning to supplement find that taking 5,000 IUs daily for a few weeks is very helpful at reducing many vague symptoms that they often never connected to poor nutritional status. You can ask for the blood test to be done; you should also ask for the pricing of the test prior to having it drawn so you’re aware of the likely expense. Manufacturers of supplements are meeting the market demand by producing combinations of D, magnesium, vitamin K, and/or iodine for patient convenience.
One warning of NOTE: vitamin K1 is vitally important in blood clotting; if you are taking a blood thinner or have been told you SHOULD take a blood thinner, including aspirin, you should discuss adding this supplement with your provider BEFORE taking it. While vital for normal body processes, vitamin K can contribute to increased clotting within blood vessels; clots are known contributors to heart attacks and strokes.
In conclusion, the general consensus on Vitamin D includes:
- Each increase of 4 ng/mL of vitamin D in the blood is associated with a 4% lower risk of type 2 diabetes.
- There is a significant and inverse relationship between blood levels of vitamin D and the risk of type 2 diabetes among a wide range of vitamin D levels and among a wide variety of populations, so that it is difficult to specify “normal” lab reference values and recommended daily dosing. Translation: The lower your vitamin D level is, the higher the risk of development of type 2 diabetes.
For further information about Vitamin D, it is recommended to ask your regular health care provider.
Here’s a link to a great study to reinforce our viewpoint: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5541280/
DISCLAIMER:
The information provided in this article and on the Joyful Heart House Calls/KetoNurses blog should be taken as basic & general information, and NOT as medical advice. All information presented by JHHC/KetoNurses should be carefully evaluated and discussed with YOUR health care professional.