Many people with diabetes, gestational diabetes, insulin resistance, polycystic ovarian syndrome (PCOS), and/or metabolic syndrome (MetS) are taking metformin, a drug that has been around for about 60 years. It is one of the oldest and safest medications used in the management of diabetes. Most people who take this medicine believe that it lowers glucose in the blood, but that is not how it works. Metformin works in 3 major ways, and these processes result in a lower glucose through INDIRECT means. Insulin and some other diabetes medications DO directly lower glucose in the blood, but metformin is not one of these types of drugs. Let’s discuss how metformin works and how it benefits people who take it.
Metformin is classified as a “biguanide” drug and is prescribed for a range of metabolic disorders as mentioned above; it is the preferred medicine and is considered the first line therapy for these conditions. It works to reduce the amount of glucose produced in the liver; it also reduces the amount of glucose absorbed through the intestines, and it improves insulin sensitivity by increasing peripheral glucose uptake and utilization. These physiological and chemical reactions occur at the cellular level, but are very effective at improving glucose and insulin utilization.
The action of metformin within the intestines is the cause of the most common side effect, diarrhea and sometimes abdominal cramping. As metformin is absorbed in the small intestine and enters the bloodstream, its direct impact is seen, almost immediately in some people. Metformin acts to stop absorption of excess glucose and this increased glucose within the small intestine exerts a laxative effect, resulting in diarrhea and belly cramps. This side effect occurs in about 50-55% of people who take metformin, and is the reason that many prescribers will titrate (increase) the dosing over many weeks. Most people can adapt to the use of metformin with a slow and gradual increase in dosing, but others seem to have issues no matter how low and slow the dosing is. Also note that it can take up to 3 weeks for enough metformin to actually lower glucose levels; because its major action is within the liver, one dose is not likely to demonstrate any impact on your bloodstream today.
Gastrointestinal side effects like diarrhea and belly cramping are usually easy to overcome with very slow and gradual dose increases; I have seen prescribers use a variety of schedules and dosing recommendations. Some work for some people, while others do not. My suggestion is this: if you have GI symptoms related to your metformin use, ask your prescriber about a slower titration schedule. I often work with clients who increase dosing over 6-8 weeks for optimal results with minimal side effects. Other tips that can be helpful:
- Eat with metformin dosing, no more than 5 minutes between food & medicine
- Take metformin IN BETWEEN bites of food at a meal
- Take metformin near bedtime with supper or small snack
- Some people find a multi-strain probiotic helpful
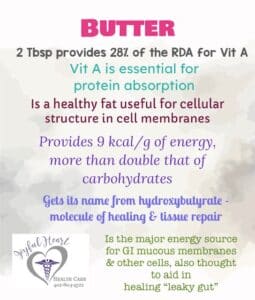
- Avoid using MCT or coconut oil within 2 hours of metformin dosing
- Ask pharmacy about switching brands of metformin
- Ask prescriber for extended release formula as these offer less impact on the gut
In addition, taking metformin can lead to a RARE and very dangerous side effect called lactic acidosis. In my 10 years as a prescriber, and after having hundreds and hundreds of patients on this medication, I have only seen lactic acidosis begin in one patient; I immediately stopped the metformin, and retested the Complete Metabolic Panel (CMP) which came back normal. Lactic acidosis is an accumulation of excessive acid due to a problem with the body’s metabolism of lactic acid, induced by certain medications or the body’s response to a medication; lactic acidosis is more likely to occur in people with impaired kidney function. It is the major reason that prescribers are encouraged to perform lab tests, like a CMP before and after starting metformin. Lactic acidosis cannot be overcome or treated with gradual dosing increase; in this particular instance, metformin is listed as an allergy on a patient’s chart and never prescribed this medication ever again. Lactic acidosis can be fatal; however, please note that this side effect is extremely rare. (FYI: Lactic acidosis is NOT the same as ketoacidosis.)
In addition to GI side effects & lactic acidosis, metformin may also contribute to kidney stress; it is sometimes very difficult to determine if the diabetes itself is causing the kidney disease, or if it is the medication. When this confusion occurs, many mainstream medical providers will stop the metformin and perform a trial of other medications to see if kidney function improves. This method sometimes works, but sometimes it does not help. Using our low carb nutrition plan will significantly lower glucose and reduce the stress on the kidneys, often reversing diabetes and kidney disease. Even if metformin contributes to mild kidney stress, it is often continued because of the risk/benefit consideration: metformin MIGHT be contributing to kidney stress, but we KNOW elevated glucose causes kidney stress and ultimately kidney failure; it is why so many patients with diabetes end up on dialysis. So, even if your kidneys begin showing signs of injury, it is often seen as a beneficial medication. Some providers will often suggest a lower dose or less frequent dosing regimen; talk to your provider to share your specific concerns and ask questions about your specific health condition. Kidney stress from the disease AND the meds can be a great reason to keep your lab tests up to date; always ask about your GFR, BUN and creatinine levels so you can be an informed patient.
Recently, experts have begun to warn about the risks of vitamin B12 levels falling due to metformin use. While it is a risk, there is currently no organization or expert that has released guidelines or recommendations for monitoring B12 levels in patients who take metformin. So, this responsibility rests with each individual patient. One of the earliest signs of B12 deficiency is fatigue, and so it’s usually easy to justify the lab test for insurer; the main reason providers won’t order extra tests is insurance regulation. Another obstacle is that by the time the B12 level has fallen below normal, the patient often has more problems that have developed. Some low carb experts are beginning to start their patients on a good quality B complex vitamin, no matter the blood level. If you have seen any of my videos or read my blog articles, you’ll know that I typically recommend a methylcobalamin for the active B12 ingredient, instead of the more-common cyancobalamin. Also note that B12 is poorly absorbed and utilized when taken alone; it needs multiple co-factors, like B3, B6, & folic acid for optimal absorption and use, thus the reason most low carb experts recommend a B complex vitamin, instead of the single B12.
As you can see, pharmacology is a complex science, especially in the context of abnormal metabolism, such as what occurs with metabolic disorders like diabetes and insulin resistance. While I do understand that learning all this information can seem daunting and overwhelming, it is VITAL for each person taking medicines to learn all you can about the medicine and its impact on your body.
What about metformin and other medicines? I strongly encourage you to use a reputable website to look for drug-drug interactions, specifically between metformin and other medicines. I will discuss only a handful of issues here. First of all, we KNOW that metformin ALONE does NOT contribute to abnormally low glucose levels – remember, it works in the LIVER and the GI tract, not in the bloodstream. However, certain combinations of anti-diabetes medicines CAN change the impact on blood glucose. For example, we know that insulin is used specifically to directly lower glucose in the blood; when combined with metformin, metformin IMPROVES insulin sensitivity and because of this action, metformin CAN cause a lower glucose than taking insulin ALONE. Read this sentence again:
When combined with metformin, metformin IMPROVES insulin sensitivity and because of this action, metformin CAN cause a lower glucose than taking insulin ALONE. Other anti-diabetes medications can also interact with metformin, resulting in this “synergistic” effect – drastically lowering glucose to unsafe levels.
Keep in mind that the lab reference range for glucose is 60 -100 mg/dL (3.3 – 5.5 mmol/L). These levels are considered NORMAL glucose readings without addition of medication. We prefer for fasting glucose levels to be less than/around 85mg/dL (4.7 mmol/L), because numbers lower than 85 (4.7) tend to show us that insulin and glucose are working more appropriately than when numbers are higher. When patients begin taking anti-diabetes medications, glucose often falls quickly, resulting in feelings of hypoglycemia – even when glucose levels are within this 60-100 (3.3-5.5) range. This phenomenon occurs because the liver and the body have become accustomed to your higher/abnormal glucose readings. All anti-diabetes drugs, including metformin, can contribute to these feelings of low glucose. It is imperative that you check glucose when experiencing these symptoms so that you know the appropriate action to take. If your glucose level is NORMAL, 60-100 (3.3 – 5.5), and you are only taking metformin, the only action that may be needed is to have your normal meal. If you are shaky, nervous, trembling, and have a headache, check your glucose, PRIOR to deciding to treat a “low glucose.” If these symptoms occur in the presence of NO medication (or metformin ONLY) AND normal glucose levels, most low carb experts recommend having your usual low carb meal or some salty broth and waiting for these symptoms to subside. Once the liver and the brain learn to respond more appropriately to your new low carb lifestyle, these symptoms disappear.
If you experience these symptoms while taking medication that DIRECTLY lowers glucose, always check glucose level and treat accordingly with glucose tablets. Keep in mind that 1 gram of glucose will raise glucose about 5 points, give or take; it is no longer accepted practice to consume candy bars, soda or sugared orange juice to raise glucose because these items cause such a wide variety of responses based on the amount and speed consumed. If these food items are consumed in response to a low glucose level, the body’s response can become a terrible day of fighting high glucose levels, interfering with normal physiological responses as well as an emotional & tiring rollercoaster for the remainder of your day. If you take glucose-lowering medication, it is advisable to purchase glucose tabs at the pharmacy and keep them with you and easily accessible all the time.
The maximum dose of metformin that is approved by the FDA for use in the US is 2500 mg daily, and it is usually in divided doses. Some prescribers will “max out” the dose and write the prescription something like this: metformin 500 mg tabs: take 2 tabs morning and night, and 1 tab at lunch. Other prescribers simply write for 1000 mg twice daily. Many prescribers will start metformin at 500 mg, planning to increase dose over time to help minimize GI side effects; sometimes the providers forget to go back and increase the dose. If you have been taking the minimally effective dose of 500 mg daily for a long time, it may be a good idea to ask your medical provider about a possible increase.
Because metformin does NOT directly lower glucose and its major impact on health is improving insulin sensitivity, most low carb providers will not lower metformin dose or stop prescribing metformin when your hemoglobin A1c or your glucose fall into more normal ranges. We typically continue this particular medication, even when glucose numbers are more normal, because of metformin’s significant impact on improving insulin sensitivity; metformin is helping your liver learn to metabolize glucose much more efficiently. Why would you suddenly want to stop teaching your liver about your new way of eating? Some providers may lower the dose, but continue some metformin; some will want to stop it because they may not understand its direct action does not occur in the blood. Most low carb providers that understand the actions of metformin typically continue this medicine until the A1c remains around 5 for 6 months to a year. When metformin doses are lowered or the medicine is stopped completely, it can take 2-3 weeks before you see any change in glucose levels; glucose levels usually do increase when meds are lowered or stopped, but be aware that the method and action of metformin cause a much slower response than say insulin or sulfonylureas.
Other medicines are often stopped or significantly lowered immediately upon beginning low carb eating; it is VITAL that your provider be kept “in the loop” with regards to your glucose levels, medications, and low carb eating. Most of them have NO idea that our way of eating AND your glucose-lowering meds will put your very life at risk if medications are continued at high doses, typically used to treat very high glucose levels caused by VERY high carbohydrate intake. Call the provider’s office every single day if needed. Fax glucose records to them daily. Ask specifically about medications BY NAME when your glucose is within normal range. And keep in mind this one fact: we do NOT treat NORMAL glucose levels. Even prescribers get busy and overlook medication action sometimes. Be very specific with your questions. Example questions:
- Should I keep taking 80 units of Lantus daily with my glucose level at 96 (5.3)?
- Is it dangerous to keep taking my 3 meds (name all 3) with a glucose level of 104 (5.7)?
- I’m taking metformin and (name other med) and my glucose today is now 100 (5.5); what should I do?
As with any health problem or medication, ALWAYS consult your health care provider for more specific information. This blog article is provided for information only and should NOT be taken as medical advice. Your health care provider knows the most about you and your health, but most of them know very little about low carb nutrition. You may have to help them understand that you are eating healthy meat, fats, and veggies, and only skipping non-nutritious calories that raise your glucose. You may have to present them with logs and records of your glucose levels for them to believe you. You may have to help teach them the simple science of low carb nutrition and its impact on your glucose levels. You may ultimately have to make some of your OWN decisions if you believe your safety is at risk. BUT always keep your provider aware of what is happening.
NOTICE: This content is for informational and educational purposes only. It is not intended to provide medical advice or to take the place of medical advice or treatment from a personal health care professional. All viewers of this content are advised to consult their own qualified health professionals regarding specific health questions. Neither KetoNurses or the publisher of this content takes responsibility for possible health consequences of any person or persons reading or following the information in this educational content. All viewers of this content, especially those taking prescription or over-the-counter medications, should consult their physicians before beginning any nutrition, supplement or lifestyle program.