Recently, another health care provider mocked my use of the phrase, “improving the health of my patients”, saying that it’s vague and not measurable.
Her comments gave me pause, because the goal of every nurse I’ve ever met has been to help people improve their health. Ask any nurse why he or she became a nurse, and you will hear a variety of ways people say it. We nurses help people get well, better, or over a health obstacle. How is that measured?
First and foremost, there are many parameters used by health care providers to measure health. With diagnoses of diabetes and hypertension, we measure glucose and blood pressure, respectively. But we often have difficulty quantifying how people feel when they lower their glucose or blood pressure. When patients return for follow-up and I’m able to tell them their hemoglobin A1c dropped from 8.9 to 6.4 after weeks of diet changes and effort, people are thrilled. They grin from ear to ear. They clap. They shake a fist in the air. They “high five” me. Some even do a “happy dance.” What is measurable here? Yes, the glucose levels are numerical and easy to track. But how does anyone put a scale on happiness or joyfulness? Can the idea that diabetic complications no longer pose a looming hazard to health be measured? How is relief quantified when kidney damage has improved?
These feelings are not measurable, yet they are extremely evident in behaviors and attitude. Patients who work toward improving health exhibit gratefulness that good instruction is provided; is that gratitude measurable?
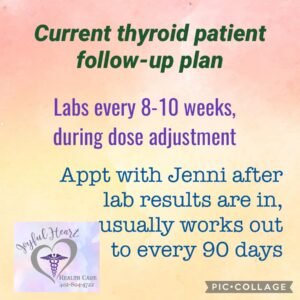
Measures are important in health care. Measurements of pulse or blood pressure provide vital information to us who render the care. I decided that some of you might be interested in knowing what measures we use for certain conditions so you can track your own progress over time.
With diabetes, one of the most important measures is glucose, of course; in addition, the hemoglobin A1c that tells us the average glucose levels over the past 90-100 days provides a good correlation to patient effort in managing the condition. While mainstream medicine will say that “good” diabetes control occurs when the A1c is around 7, many studies have shown that diabetic complications occur when the A1c runs higher than about 6.2 or so. Normal A1c levels run around 5 or less; why should people diagnosed with diabetes be forced to run glucose levels so high that we KNOW organ damage will occur? Is that going to help patients “improve their health”?
Elevated blood pressure is often associated with diabetes because high glucose levels cause thick, sticky blood; demanding that the heart pump thick, sticky blood to an overweight body will eventually result in high blood pressure. The heart will pump harder and with more force to move thick “syrupy” blood through tiny blood vessels, resulting in higher and higher blood pressure readings. When blood pressure increases, the heart muscle becomes compromised and weaker. Daily demands on the heart that continually exceed it’s designed capabilities can contribute to a multitude of vague symptoms which are not measurable, including headaches, fatigue, nausea, dizziness, or even mild swelling. While most of these symptoms have no quantifiable scale, patients will describe how much better they feel once blood pressure is lowered. While blood pressure is measurable, the feeling of lower and healthier blood pressure is described by patients as “improved health.”
If blood pressure remains untreated or poorly managed, heart failure and/or kidney damage begin to occur. Highly pressurized blood flow moving through the kidneys will damage the fragile vessels, reducing the filtering ability of the kidneys. Elevated glucose can also damage these tiny vessels, resulting in inflammatory responses by the body that are designed to patch and repair damage – but this natural response by the body can result in blood vessel blockages. Think scar tissue.
In this photo below, notice that cholesterol is serving as the patch, relating the damage to the blood vessel. Cholesterol isNOT the cause of clots; it’s part of the damage control/repair team of the body. In summary, how do we measure “improved health”? How can we quantify patient comments when they express gratitude for how they feel? How can we count the number of clinic visits these patients will NOT have? How do we track hospitalizations that do NOT occur for these patients? What evidence do we see when ER visits are no longer the norm for people with “normal” glucose or blood pressure? We can’t. But these numbers ARE real. These people ARE changing their lives and IMPROVING HEALTH!
If you want to take charge of YOUR health, email us for more info at KetoNurses@gmail.com