DISCLAIMER:
The information provided in this article and on the Joyful Heart & KetoNurses blog should be taken as basic education & general information, and NOT as medical advice. All information presented by Joyful Heart & KetoNurses should be carefully evaluated and discussed with YOUR health care professional.
One of the most frustrating battles many of my clients face is the higher fasting glucose every morning; even after months of a low carb way of eating, the fasting glucose level often remains higher than goal. In this article, I will try to explain how and why this “dawn phenomenon” occurs; we’ll also discuss some possible remedies.
Let’s review a bit of pathophysiology from “The Chaos Within”:
“In the liver the high levels of insulin, glucose, and associated inflammatory processes combine to trigger storage of glucose in the form of glycogen; once the liver has stored all it can hold and blood sugars remain high, the liver doesn’t know what to do with all the excess carbohydrate being ingested. It just keeps storing more and more. Let’s imagine that you decide to put your household garbage in the pantry, instead of taking it outside to the trash bin for collection. Keep doing this. Every time you fill a garbage bag, you pull it out of the can, tie it up, and pile bag after bag in the pantry; then you run out of room, and begin filling kitchen cabinets. Eventually, those cabinets fill as well; so where do you store it now? Over time, the garbage comes to overwhelm the entire kitchen, so much so, that normal function in the kitchen is halted. There is literally nowhere to work or accomplish cooking tasks. That’s what happens in our livers with glycogen storage. There’s room for a little glycogen, so in times of famine, the liver can release a few grams of glucose the body needs, but there’s not room for 200-300 grams of carbs per day for a lifetime.”
In metabolically healthy people, the liver is able to release glycogen any time of day or night, whenever blood levels of glucose fall below 60 mg/dL or so; this process of homeostasis, or internal balance, helps our bodies avoid low glucose and maintains adequate amounts of glucose & insulin in the body in appropriate amounts, ready for use. Overnight, while the body is burning stored energy, the liver is the main organ responsible for glucose level maintenance; since we aren’t consuming energy overnight, the glucose level can fall, triggering glycogen release from the liver in the early morning hours. Normally, there’s a measured amount of glycogen released and there’s no significant problem.
When metabolic dysfunction, insulin resistance, and/or diabetes occur, the typical internal chemical balance is threatened; over time, the process becomes quite faulty. With many years of elevated glucose, the body begins to adapt to the higher glucose levels. Glucose levels as high as 250 mg/dL can seem normal to the liver. I hear patients comment ALL THE TIME, with something like, “oh, it’s ok; that’s my normal.” Or “if I get to 150 or less, I get sick so I just like to stay high.” Neither of these statements are HEALTHY at all, and the philosophy behind these thoughts are why so many diabetes patients suffer with serious complications, including vision loss, nerve pain, heart injury, and kidney damage.
Normal glucose is normal glucose – no matter who we are, what we do, or how we think. Elevated glucose damages organs, whether it’s seen, felt, or presented to us; the damage is microscopic and continues to impact cell after cell until the entire organ is sick. Organ damage begins when glucose levels hit 120 mg/dL or so. We usually have more serious symptoms by the time an entire organ is that sick. This same philosophy occurs with glycogen storage in the liver – we don’t have any symptoms; the liver isn’t significantly damaged – YET – and so we go on with life as if nothing is wrong. All the while, the liver continues to store more and more glycogen, eventually swelling liver tissue; this damage is called non-alcoholic fatty liver disease (NAFLD). Left untreated, NAFLD will become cirrhosis and will be untreatable; there is no mainstream medical treatment for NAFLD at the time of this writing. However, a low carb or ketogenic eating plan can REVERSE fatty liver, typically in 3-6 months. YEP, you read that right!!
Cutting carbs and processed foods will significantly lower the stress on the liver rather quickly; I’ve seen blood levels of liver enzymes normalize within 3 months of low carb eating. I’ve seen triglycerides fall from 7,000 mg/dL to 90 mg/dL in 9 weeks. Both of these events were the result of cutting carbs and getting glucose levels down. However, neither of these tactics usually impact that fasting glucose number, no matter how hard we try.
Dawn phenomenon occurs simply because the liver believes it is doing its job properly; it releases glycogen in response to falling glucose, even if it’s NOT less than 60 mg/dL. Once glucose climbs, the liver, the brain, the entire body “adapt” to the higher levels, often with such gradual symptoms, that people never notice the fatigue, the muscle aches, the headaches, the occasional lightheadedness, the occasional tummy ache, or the numbness/tingling in hands/feet. As the body adapts to these higher numbers, the liver also adapts, secreting stored glucose whenever it perceives a fall. For you, it might happen at 200 mg/dL, for someone else, it may happen at 160 mg/dL. The specific number is not the important detail here; rather, the fact that the liver will continue trying to keep your glucose WHERE IT USED TO BE is the important thing to remember. Your liver truly is following instructions that you taught it.
Once we cut carbs, of course glucose falls; however, the fasting glucose will fall much more slowly than post-prandial (after meal) glucose readings. Don’t worry and don’t spend energy stressing over this fact. Just keep on working at it; some people have a LOT of glycogen stored in the liver. Until the liver gives it up, glucose readings are likely to be higher than we like, first thing in the morning.
Patients who take insulin to help manage glucose levels are at higher risks of battling dawn phenomenon sometimes because insulin’s job is to lower glucose. But if the body has become adapted to higher glucose levels, the liver will battle with the insulin, releasing more glycogen, trying to keep that glucose where it has been. Only with time, does the liver learn better behavior. It really just takes time.
WARNING: If an insulin-using diabetic chooses to go on a low carb eating plan, serious dangers abound. It is VITAL to LIFE to make sure your prescriber is fully aware of your decrease in carb intake; even if they don’t agree with your way of eating, they have a moral & legal obligation to adjust your medications to accommodate the food you’re eating. If they won’t work with you BEFORE you start cutting carbs, then you must call their office DAILY with your glucose readings and ask, SPECIFICALLY: “I am on this medicine (and that medicine) but my glucose reading today is ?? Do I need to continue BOTH/THIS medicine with glucose this low?” While they do have your records, the staff is UNLIKELY to pull your entire chart for the phone message; your LIFE depends on YOU being VERY specific with your report and your question. I cannot stress enough that YOU MUST BE PERSISTENT with clinic contact!!
SO, is there anything we can do about dawn phenomenon.
Yes, there are several strategies that can help, but there isn’t a tried & true definite treatment for DP. Time is the best healer but cutting carbs to less than 20 grams per day is key. Some people will try 100 g/day; others may swear by 50 g/day. But honestly, the only way that I see real success and decreased frustration is to keep carb intake as low as possible. Remember that carbohydrates have never been deemed essential to life or health by any national or worldwide organization or agency. We don’t need them; the body can produce glucose from any carbon, hydrogen and oxygen molecules. WE DO NOT NEED TO CONSUME CARBS AT ALL.
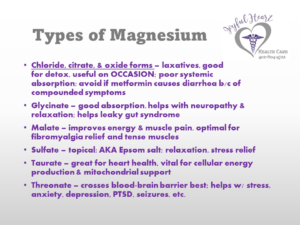
Some people find that metformin, berberine, or inositol improve DP; these medicines are believed to be of benefit because of their impact on insulin resistance. Because neither metformin nor berberine lower glucose directly, and because they work primarily in the liver improving insulin resistance, these medicines reduce the amount of glycogen released by the liver, especially when one dose is taken in the evening. Keep in mind that these metformin and berberine should NOT be taken together since they work in the same pathways and pose similar risks. Inositol can be taken with berberine or metformin; it works differently. Always seek the advice of your prescriber before taking medicines, herbs, or supplements. (Yes, I realize they probably don’t really know, but you STILL MUST ASK.)
Some low carb experts recommend splitting the long-acting insulin doses into 2 or 3 injections per day, to help reduce the risk of glucose falling too low in the early morning hours, triggering the liver’s response; this strategy should also be discussed with your prescriber.
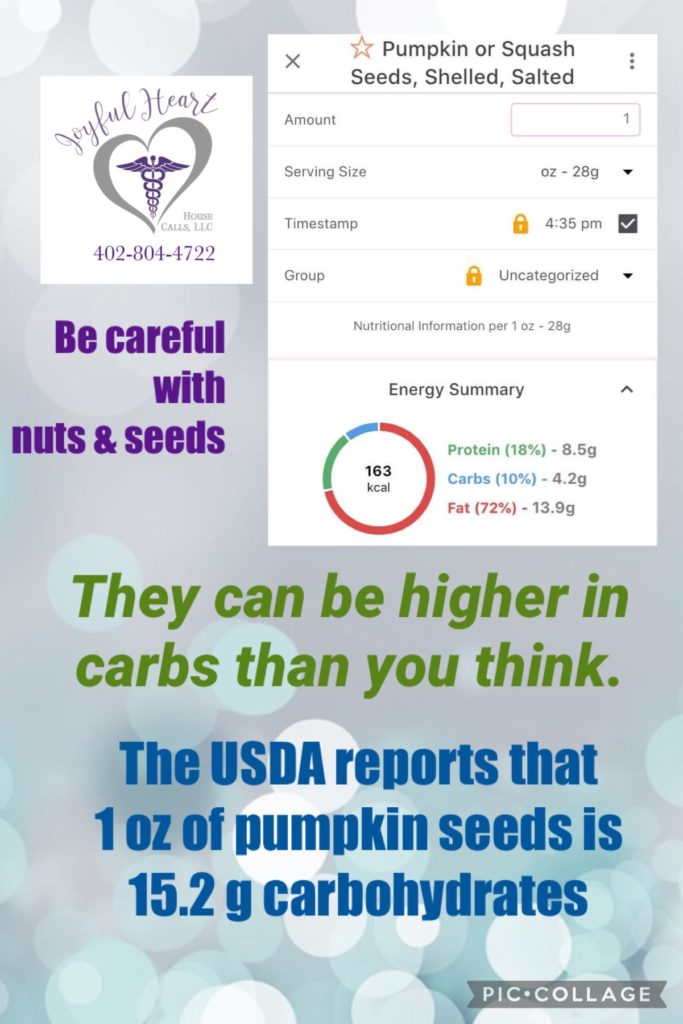
Some people find that a small bedtime snack is quite helpful at reducing DP impacts. Some people find no change at all. Some people find that a protein snack is more helpful, while others find that a fatty snack results in lower FBS. These strategies may require some patience and trial & error to determine impact on YOUR specific glucose reading. Some people will choose cheese, egg, or bacon as the evening snack, but others may use cream cheese or even avocado. Be careful with avocado; it can contain a LOT of carbs.
During daytime hours, teach your body to go longer and longer between meals; the liver remains highly stressed when we constantly bombard it every 2-3 hours with high carb meals and snacks. It literally NEVER gets a chance to rest or recover from the previous intake before it begins processing the next batch of carbs. Try to keep daytime meals/snacks at least 5 hours apart; try to get at least 13 hours from supper to breakfast/first meal of the day. Both of these time frames allow rest for specific liver processes that can significantly help with insulin resistance. (Keep in mind that it may not be SAFE to attempt this particular strategy if you inject insulin. If you’d like to schedule an appointment with me, you may call Joyful Heart Health Care at 402-804-4722.) Teach your liver to do what YOU want it to do, and it will!!
Lastly, keep in mind that having normal glucose levels throughout your day is MUCH more important than seeing a normal FBS. I understand that you want a lower HgbA1c than you’re getting right now, but given time, that DP will eventually disappear. The body WILL heal; the liver will learn how to respond more efficiently. If your glucose levels through your day are mostly running 70 – 110, then take a deep breath and chill. Don’t worry about the fasting glucose level. Retrain your liver to manage your glycogen stores more efficiently, but be patient. Let the miraculous body you have do its thing and heal itself. It can. It will.
DISCLAIMER:
The information provided in this article and on the Joyful Heart Health Care & KetoNurses blog should be taken as basic & general information, and NOT as medical advice. All information presented byJoyful Heart & KetoNurses should be carefully evaluated and discussed with YOUR health care professional.