Oftentimes, a patient will come in or someone will post on Facebook that new symptoms have occurred and evaluation is now needed. Today’s blog article will discuss some of the most common symptoms that bring patients in for diagnosis and treatment. We’re going to give 2 fictitious patients a run through a visit with me: Dick and Jane will be our patients today.
Jane is a 43 year old female, who comes in with a new complaint of “just tired all the time”. She occasionally takes a multivitamin, but not much else. She reports no previous major medical history, but does report that her dad had a stroke at age 61 and is now disabled because of weakness on the left side. She reports that her mom does have thyroid problems and takes some meds for it but she’s not sure of the exact problem. During a review of systems, she also reveals that she is beginning to have trouble sleeping through the night, her hair seems brittle, and she’s only having 2 bowel movements a week. She reports mostly normal menstrual periods, with occasional skipping of a month. She says over the past 3 years, she’s probably missed 3-4 periods; all pregnancy tests were negative. She also admits to very slow weight gain over the past 5-6 years; she says she used to weigh around 130 for most of her life. During the physical exam, Jane appears pretty normal except for these findings: weight is 214 lbs (height is 5’4”), her skin appears quite dry and even scaly on her arms & legs, very sluggish bowel sounds in all 4 quadrants of her abdomen, and her face just appears fatigued. She denies problems with depression, but is beginning to think that she might be depressed because many mornings upon awakening, she is exhausted and dreads getting out of bed. She requests lab work to help identify what is going on.
Dick has made an appointment today because of several issues that don’t seem to be linked. Although he’s done some internet research, the symptoms he’s experiencing aren’t really connected, he reports. He is somewhat tired, but not every day, and certainly not all day; fatigue just seems to hit randomly, requiring a nap to get through the rest of his day. He does report a history of mild elevated blood pressure for which he sometimes takes his Lisinopril – averages about 3-5 days a week. He also reports a recent onset of an annoying dry cough without fever or sinus/allergy drainage – which he does have a history for. He says he had a biometric screening done several weeks ago at work and brings in a copy of those results for review. His vital signs: heart rate 84, BP 168/108, O2 sat of 90%, temp 98.5, respiratory rate 22. During the physical exam, these abnormalities are noted of this 54-year-old male: waist circumference is 52 with very protuberant abdomen (no distention, more of a “beer-belly” appearance), lung sounds are clear, but deep breathing triggers his cough, and an extra heart sound (S3) is noted. In addition, he exhibits trace bilateral pedal edema, but normal pedal pulses. In review of his biometric results, he has a random glucose level of 186, LDL 201, HDL of 32, Total cholesterol 259, and Triglycerides of 276. He says they offered health coaching to him, but he hasn’t decided whether to do that or not; he says he wanted to be seen for good physical first.
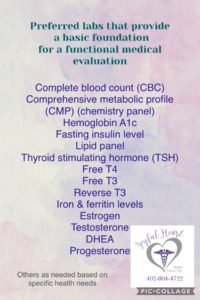
During Jane’s visit, we decide to obtain some lab tests; drawing a Complete Blood Count (CBC) will help us recognize a possible anemia or subtle infection she may have. A CMP (compete metabolic panel) will tell us about her electrolyte balance, kidney and liver function, while thyroid studies will help identify thyroid problems. In addition, we obtained a urine dip and a hemoglobin A1c in the office. We discussed a variety of home remedies and OTC medications/supplements that can help improve fatigue in general, until we can review lab results. Jane is much relieved to hear that B complex vitamins, Vitamin D, and magnesium are easy to access and often improve fatigue in many people. She prefers to use supplements and lifestyle changes if possible. She leaves the clinic feeling better about her outlook and has an appointment for a 2-week follow-up.
Recommended foundational labs for a functional medicine workup
In reviewing Dick’s biometric results, we discuss the likelihood that he has diabetes; he agrees that he’s thought the same for a while now, but never tested for it. Reports his mom was diagnosed with Type 2 DM as an adult many years ago and has now progressed to insulin use with possibility of dialysis in the near future. He expresses great concern over dialysis and states emphatically that he does NOT want to go down that road at all. We draw similar labs on Dick as Jane had; we also get a BNP (brain natriuretic peptide) level and an office UA and A1c before sending him home with an appointment Friday for review of all the results; we also schedule an appointment for an EKG and an echocardiogram – both are tests to help determine cardiac muscle injury. The BNP is a blood test that helps us determine possible weakening of the heart muscle that often accompanies poorly controlled blood pressure and diabetes.
When Dick returns for his Friday appointment, we first begin with review of the abnormal test results, beginning with the mild abnormalities and working our way toward the more serious problems. His urine is mostly normal, except his protein which is mildly elevated and specific gravity is 1.030 which often indicates poor water intake as it shows high urine concentration. Elevated blood pressure and diabetes will both contribute to protein spilling into urine – each for different reasons. High blood pressure will cause it because of the force of blood being pushed into the kidneys and the tiny little blood vessels literally burst sometimes. Diabetes will cause protein to spill into urine because of tiny little “beaver dams” in blood vessels – thick, sticky, syrupy blood causes tiny components of glucose, triglycerides, and inflammation markers to bunch together, forming a bit of a “beaver dam” inside blood vessels. When these blockages occur, protein is not filtered properly through the kidneys’ processing system and it spills out into urine. Since Dick has both high BP and diabetes (DM2), it’s difficult to pinpoint his cause of protein in urine. Moving along, his A1c is 7.8, meaning his blood sugars are averaging around 200 mg/dL. Review of the CMP reveals slightly elevated AST (a liver enzyme), slightly elevated BUN (kidney function test), but normal creatinine, and his BNP is somewhat elevated at 278 pg/mL. Normal BNP is less than 100; CHF (congestive heart failure) is most likely over 400. His EKG is mildly abnormal, but shows no significant electrical problem with his heart. However, the ECHO (echocardiogram) does indicate weakened heart muscle, with an ejection fraction of about 45%. Normal EF is approx. 50-65%, meaning that during each beat/contraction of the heart, approximately 65% of blood inside the heart is pumped out during that one beat. Remember, Dick, that the heart’s 4 chambers each contain blood and only the ventricles (the 2 bottom chambers are pumping blood OUT of the heart during that beat, and the RIGHT ventricle is pushing blood to the lungs, while the LEFT ventricle is pushing blood out to the body for use by its cells. The EF is calculated based on how much blood is leaving the LEFT ventricle during one beat. You don’t want the EF to be 100%, or your heart would not be able to keep working properly. It should push out 50-65% of its contents during any given beat or contraction. When the EF falls too low, it signals that the heart muscle is trying to beat stronger and stronger to push out the blood for the body to use.
Dick expresses a bit of confusion and so we continue to explain. Have you ever been to the gym to work out? What happens when you start working out? Lifting weights? Your biceps get bigger and stronger, right? But the heart muscle is NOT like skeletal muscle at all; when the heart muscle works more and harder, it gets weaker – NOT stronger. Asking the heart to pump thick and stick blood to an overweight body is not healthy and will cause organ damage – in this case – heart muscle injury, kidney injury; the mild liver damage, likely non-alcoholic fatty liver disease (NAFLD) is related to long-term insulin resistance/high carb intake/elevated glucose & triglycerides. Dick says he’s beginning to understand how all of these health problems are related to one another and now wants to know how to reverse this damage. He says he’s determined to improve his health. So, looking at Dick’s chart, and reviewing everything with him, we list the following as current medical diagnoses in his record: hypertension, type 2 diabetes, congestive heart failure, hypercholesterolemia, proteinuria, & NAFLD. Dick asks if all of this can be reversed without medications and is leery of taking home a shoebox full of meds today. We review the most important problems of high BP and heart injury and decide that these do need some medication, at least for now; Dick agrees to start on BP meds and a diuretic to reduce the workload of the heart. After much discussion of diabetes meds, he agrees to start on metformin which does not directly lower glucose, but aids in liver health and insulin resistance. He agrees to start other meds if needed, but wants a real chance with nutrition changes to see if he can eat better to get healthy. We agree on a monthly visit schedule for a while, just to help and support Dick through these life-changing diagnoses; he came in for one visit and now has multiple life-altering diagnoses with multiple meds and a whole new outlook on life.
Jane is back today for her 2-week follow-up and review of her lab results. Most of her results are pretty normal; her random glucose is 146. Her thyroid levels are within normal ranges, but just barely. Her TSH is at the very upper end of the normal reference range; her T4 is pretty normal, but her T3 is right on the lower end of normal. Her liver enzymes are all slightly elevated, but not very high at all. Her A1c is 6.3; her urine is pretty normal, except her specific gravity is also 1.030. It is determined that Jane has subclinical hypothyroidism, pre-diabetes, and likely NAFLD/insulin resistance. Much of our discussion with Jane is similar to our meeting with Dick, except the heart failure topic. We discuss starting her on thyroid meds, vitamin D and magnesium regularly with follow-up thyroid labs in about 6-8 weeks because it can take many weeks for thyroid hormone levels to improve. Jane is thrilled to have some answers to her symptoms and agrees to start on thyroid meds. We caution her to take thyroid meds, completely alone, with no other food/med for at least 30 minutes because thyroid meds bind easily to caffeine, calcium, and many chemicals/foods. Jane agrees and leaves with hope that she will feel better soon, but she also asks about her sluggish bowel movements and wonders what she can do to become more “regular”. We discuss many possible remedies for constipation, including various brands of colon cleansers, OTC laxatives, and foods that can trigger faster GI motility. She agrees to find something when she picks up the thyroid prescription at the pharmacy. She schedules her follow-up for about 6 weeks out.
Both of these patients teach us a lot about general health. First, we all minimize many of our symptoms from time to time, thinking it’s just growing older, being too busy, or just not resting well. But we should always take note of even mild/vague symptoms that don’t improve after a week or so. Secondly, there are many reasons for fatigue, and if a good evaluation by a provider reveals no likely source, trying vitamins or supplements might help boost energy levels. Thirdly, there can be many, many mild abnormalities going on internally, that we cannot see, feel, or easily identify without lab tests. And lastly, both patients had some carbohydrate intolerance, as evidenced by even mildly elevated glucose levels, weight, and missing menstrual periods.
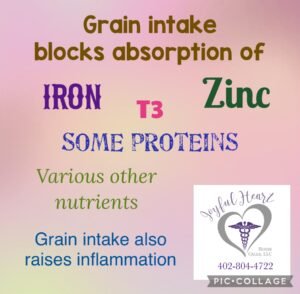
I am a firm believer that high carbohydrate nutrition has led us all down a path to poor health, vague symptoms, and a variety of chronic health conditions. Look at nutrition labels for any processed food; very little actual nutrition, yet agencies PUSH us to eat that stuff. Why? Because Big Food has paid billions of dollars in advertising and donations to organizations like ADA, AHA, AMA, etc. There was absolutely NO scientific evidence that our bodies EVER needed carbohydrates; if so, they would be considered ESSENTIAL to our health, but carbs are NOT essential. The body will make any necessary glucose it needs from proteins and fatty acids. Start eliminating carbs today and reclaim your health!
Every choice we make – either for good or bad – influences consequences. What choices will YOU make this week to influence your health for the better?